Surgery or Stem Cell Injection?
 Is getting surgery or a stem cell injection for joint osteoarthritis better?
Is getting surgery or a stem cell injection for joint osteoarthritis better?
When making a healthcare decision, weighing the risks and the benefits is good.
With any treatment, one should first and foremost consider the invasiveness of the therapy.
FIRST DO NO HARM is an oath that all doctors take in accepting the license to practice medicine.
As a naturopathic physician, I constantly implore my patients to practice that oath for themselves.
Whether it be in lifestyle choices or in choosing treatments for their health problems, unfortunately, some treatments are inherently invasive.
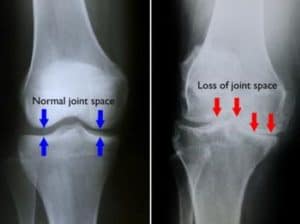
For joint arthritis, there are only two choices offered by conventional medicine.
These are pain management and surgery.
Pain management includes oral pain meds and steroid injections.
Pain medications block the pain; however, they come with addiction and side effects.
Some patients can never get off of them due to the severe withdrawal symptoms.
The steroid injections further weaken the joint as corticosteroids cause degeneration of the ligaments, tendons, and bones.
These injections have a limit to their pain relieving effects so it’s a very temporary solution.
Surgery is done in severe osteoarthritis or when a ligament or tendon is a complete tear.
The risk of surgery is like any other surgery.
Anesthesia is always a risk, especially in older patients.
There are cognitive effects of anesthesia and the more dangerous risks of aspiration and infections which can be life threatening.
As if aspirating and getting an infection is not enough, there is also the risk of blood clots, which could cause a stroke.
The benefit of surgery could be significant pain reduction.
How long it lasts is not guaranteed and varies from patient to patient.
Post-surgery, the patient must do extensive rehab, up to 6 months to one year.
Stem cell therapy is a powerful alternative to surgery and pain management.
This regenerative therapy heals the ligaments and tendons that hold the joint together.
There are three sources of stem cells: bone marrow, fat aspirate (both of which are taken from the patient), and umbilical cord and blood.
Umbilical cord stem cells are the most effective o
ut of the three types of stem cells.
Bone marrow and adipose tissue produce a variable product, depending on the patient’s age.
The older the patient is, the fewer stem cells the final product will have.
Also, umbilical cord stem cells travel further so that sometimes a patient will experience an improvement in their vision or their ankle stops hurting following a knee injection.
These naive and primitive cells divide faster, differentiate more, and have stronger anti-inflammatory effects than adipose and bone marrow stem cells.
What are the risks and benefits of stem cell therapy?
The injection itself takes 5 minutes, there is no anesthesia involved, so no risk of cognitive decline or aspiration.
There is no risk of blood clots or infection.
No physical therapy is necessary, as the pain will decrease within 24 hours, and the patient can work out the next day.
The benefits last just as long and maybe longer than surgery.
There are no physical risks to receiving stem cells, as the cells are immune privileged.
The cost of a stem cell treatment will most likely be less than that of surgery.
No PT or MRI will be necessary which saves the patient significant co-pays.
When deciding what treatment to do, the first question one must ask themselves is how invasive will the therapy be on the body.
If the benefits and costs are similar, the risks and time to heal should be the important decision-makers.
The stem cell treatment wins the contest regarding risks and time to heal.
For more information, book a free consultation here.
